| 05.a • | Trauma team roles |
> Section 10.a.ii
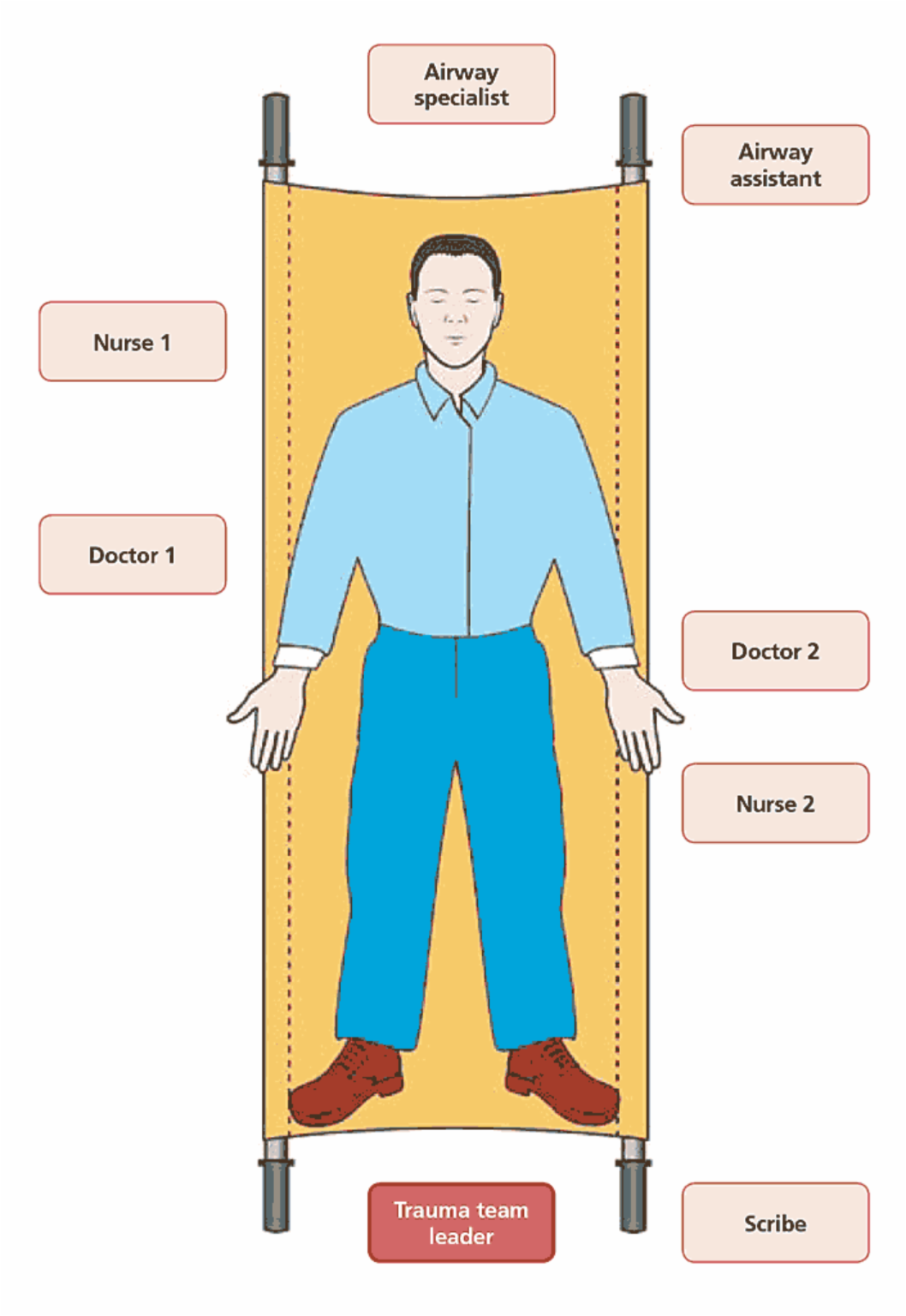
Trauma team roles
Trauma team leader
- consultant in MTC
- ST5 or above in TU
- controls and manages the trauma team resuscitation
- makes decisions in conjunction with specialists
- prioritises investigations and treatments
- is responsible for all handovers and transfers
- follows checklist
> Section 10.a.i
Trauma team checklist
Before patient arrival
- ensures trauma team activated
- appoints scribe (preferably additional team member)
- ensures correct PPE and identification worn
- ensures CT notified
- ensures team members ‘book in’ on ED documentation
- introductions and roles assigned
- ensures tranexamic acid ready (if needed)
- ensures blood products ready (if activated)
- ensures theatre ready (if right turn resus)
- briefs team
- starts the clock when the patient arrives in the bay
Airway specialist
- communicates airway patency and issues to team leader / scribe
- ensures patient oxygenated and ventilated with no airway obstruction. Intubate when appropriate only in discussion with the team leader
- ensures cervical spine immobilisation
- it is usually appropriate for the airway specialist to talk to the patient and provide
ongoing assessment of GCS. Reassures patient on arrival, sets the scene of what is
happening and takes AMPLE history:
A allergies
M medications
P past medical history
L last meal
E everything else relevant - this role may be shared with doctor 1. Inform outcome to team leader / scribe
- considers need for endogastric tube
- arterial lines may be indicated. To avoid delay to CT this can usually be done after CT or in the operating theatre. It should not delay either
- communication with theatres role is shared with surgeon
Airway assistant
- may assist with removing patient clothes, have scissors to hand
- assists airway specialist in all airway interventions
- takes emergency airway equipment / drugs on any transfers (CT, theatre, ITU)
Doctor 1
- undertakes primary survey <C>ABC. Clearly states findings to team leader and scribe
- takes AMPLE history if anaesthetist busy, reassures patient on arrival,
sets the scene of what is happening
A allergies
M medications
P past medical history
L last meal
E everything else relevant - performs procedures depending on skill level and training. Confirms skill levels with team leader prior to patient arriving
- neurology exam needed before paralysing anaesthetic agents used
- ensures patient kept warm
Nurse 1
- prepares for trauma call with warming devices, tranexamic acid (if needed)
- prepares for the trauma call with level one run through when indicated, warmed IV fluids run through, chest drain sets out if suggested
- ensures full monitoring is applied quickly and observations fed back to the team leader
- has scissors ready – removes all clothing including underwear and store securely covers with Bair Hugger / blankets – check temperature
- prepares for transfer to CT ASAP (possibly within 10–20 minutes) and/or theatre
- helps with procedures as identified, eg. catheter, chest drain, arterial line
Doctor 2
- two peripheral lines taking 20mls of blood at same time
- bloods needed will usually include:
FBC
U&E
LFT
pregnancy test
XM 6 units (or G&S occasionally)
glucose
coag screen
venous gas (will include glucose and lactate) - orders radiology and bloods in discussion with team leader
- performs procedures depending on skill level and training and as guided by team leader.
- Confirms skill levels with team leader prior to patient arriving
- FAST scan if accredited and not delay CT
- administers drugs, eg. analgesia, antibiotics. Keeps patient warm
- undertakes secondary survey including tympanic membranes
Nurse 2
- has scissors ready – removes all clothing with nurse 1
- helps with getting IV access and sending bloods off if required, sets up intraosseus kit (ezi-IO) if no / difficult IV access
- draws up drugs / administers as prescribed
- helps with procedures as identified for nurse 2 or doctor 2
- prepares for transfer to CT as soon as possible and/or theatre
Scribe
- use ED trauma documentation
- records names, grades and specialties of all clinical staff attending, plus time of arrival
- ensures clock is started when patient arrives and is recorded in ED trauma documentation
- records all observations
- records all findings and interventions
- ensures patient wrist labels are applied (including allergy)
> Section 13.a
ED trauma documentation