The TEMPO guidance aims to build upon the teaching and practice of ATLS (8th edition) which all those involved in acute trauma care should be familiar with and is regarded as the basic standard of care for major trauma patients. All emergency departments in the Network are expected to follow the same emergency management of the major trauma patient based upon these guidelines.
| Elapsed time | Processes undertaken |
| Time 0 | Patient on ED trolley |
| Within 10 minutes of arrival to the ED | Reception/handover Primary survey and immediate interventions Establish ED monitoring Establish anaesthesia and ventilation (if required) Establish appropriate IV access, undertake venous blood gas, give analgesia +/- fluids Request immediate imaging: CT in stable patients, FAST and PXR in unstable patients Identify and transfer to trauma theatre if patient necessitates immediate damage control surgery |
| Within 30 minutes of arrival to the ED | Gain cardiovascular control Administer tranexamic acid: First bolus (if not already given) and start second infusion Any immediate radiological studies undertaken in resus complete and available for viewing Antibiotics / tetanus given Transfer to CT and start scanning |
| Within 60 minutes of arrival to the ED | Formal CT report available Images transferred to MTC and Network Co-ordination Service contacted Complete secondary survey and further treatments Further imaging undertaken, eg. limbs Tertiary specialist involvement, eg. ENT, maxfax Disposition / transition plan made |
| Within 90 minutes of arrival to the ED | Transition to final destination |
Targets for damage control resuscitation
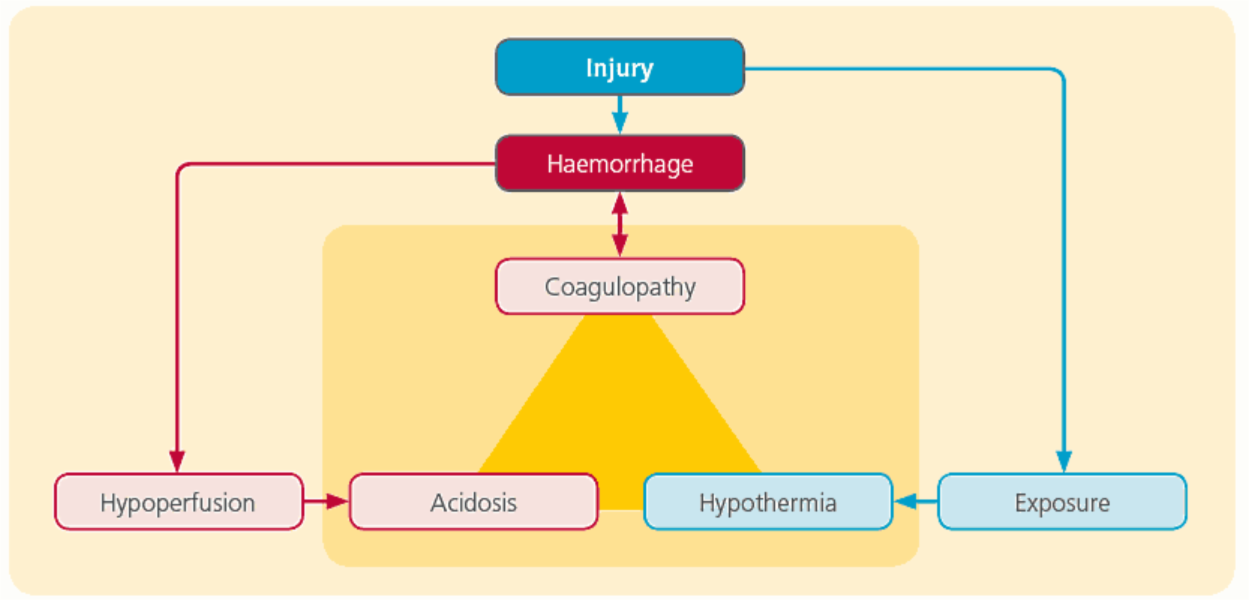
The injured patient can quickly become hypothermic, acidotic and coagulopathic in response to the injury. Damage control resuscitation aims to prevent further damage by targeting these problems.
Hypothermia
- limit patient exposure where possible
- use a forced air warming product (eg. Bair Hugger) to maintain a normal body temperature
- blood products and IV fluids should be warmed for giving
Acidosis / coagulopathy
Acidosis usually reflects hypoperfusion secondary to haemorrhagic shock. This hypoperfusion is also thought to be one of the initiators of the early coagulopathy seen in trauma patients that cannot be measured using the PT and APTT.
- control major external haemorrhage
– direct pressure
– tourniquets
– haemostatic agent (eg. Celox™) - control internal haemorrhage
– splinting fractures (femur and pelvic) - maintenance of perfusion pressure
– aiming for systolic BP of 90mmHg in those without a head injury
– aiming for a MAP >80mmHg in those with a head injury - early use of blood products
- ensure tranexamic acid has been given (both doses)
- damage control surgery, if needed