The imaging modality of choice in acute severe trauma is CT. Definition of severe
trauma is ISS >15. However, in the acute setting trauma CT may be deployed in
patients with ISS of 8–15. A list of suggested indications for whole body trauma
CT protocol is included below. In minor / moderate trauma or where one body
part is injured, the CT protocol may be tailored appropriately. Caution should
be applied regarding distracting injuries.
Acquisition of trauma CT images should be protocol driven. This enables the imaging
process to be streamlined and provide uniformity across the region. Definitive
imaging should not be delayed by other less accurate investigations1. FAST imaging
and plain film imaging may be indicated in certain scenarios, this is detailed in the
document ‘Standards of practice and guidance for trauma radiology in severely
injured patients’ published by the Royal College of Radiology1.
In pregnant patients modification of the pathway should be discussed between
the trauma team leader and radiologist. Depending upon the mechanism and
severity of injury, CT may still be the imaging modality of choice.
Transfer to CT should be rapid with minimal delay. Radiology must indicate when
the scanner is available and therefore when the patient can be moved.
The CT trauma protocols utilised in the major trauma centre are provided for both
adult (appendix 1 and 3) and paediatric polytrauma (appendix 2). Further guidance
on the use of alternative protocols is available in the Royal College of Radiology
document1.
The general principles for polytrauma imaging include:
- time is of the essence
- adequate imaging coverage
- avoid a ‘piecemeal’ approach and repeated visits to the CT department
- optimise images obtained. For example, in pelvic fractures, arterial phase imaging is crucial for assessment of arterial versus venous bleeding
- aim to keep radiation exposure as low as reasonably possible
- trauma team leader to discuss CT request with radiologist. Clinical presentation should guide most appropriate imaging
Suggested indications for CT imaging from vertex to symphysis in polytrauma2 are:
Clinical
- all adequately resuscitated major trauma patients
- all ventilated trauma patients
- spinal injury with neurological compromise
- reduced GCS (excluding isolated head injury)
Mechanism
Mechanism may not be a reliable guide to injury. The list below should act as a guide in conjunction with clinical signs.
Blunt trauma:
- ejection from vehicle / thrown from motorbike
- motor vehicle fatality in the same passenger compartment
- motorbike / bicycle / pedestrian hit by car at ≥20mph
- prolonged extrication time (>20mins)
- crush injury to thorax / abdomen
- fall >3m (10ft)
Penetrating trauma:
- blast injury (explosion / bomb)
- gunshot wound
Reporting:
All trauma CTs should be reviewed whilst the patient is on the table, particularly
for foci of active bleeding. Notify the relevant clinicians promptly.
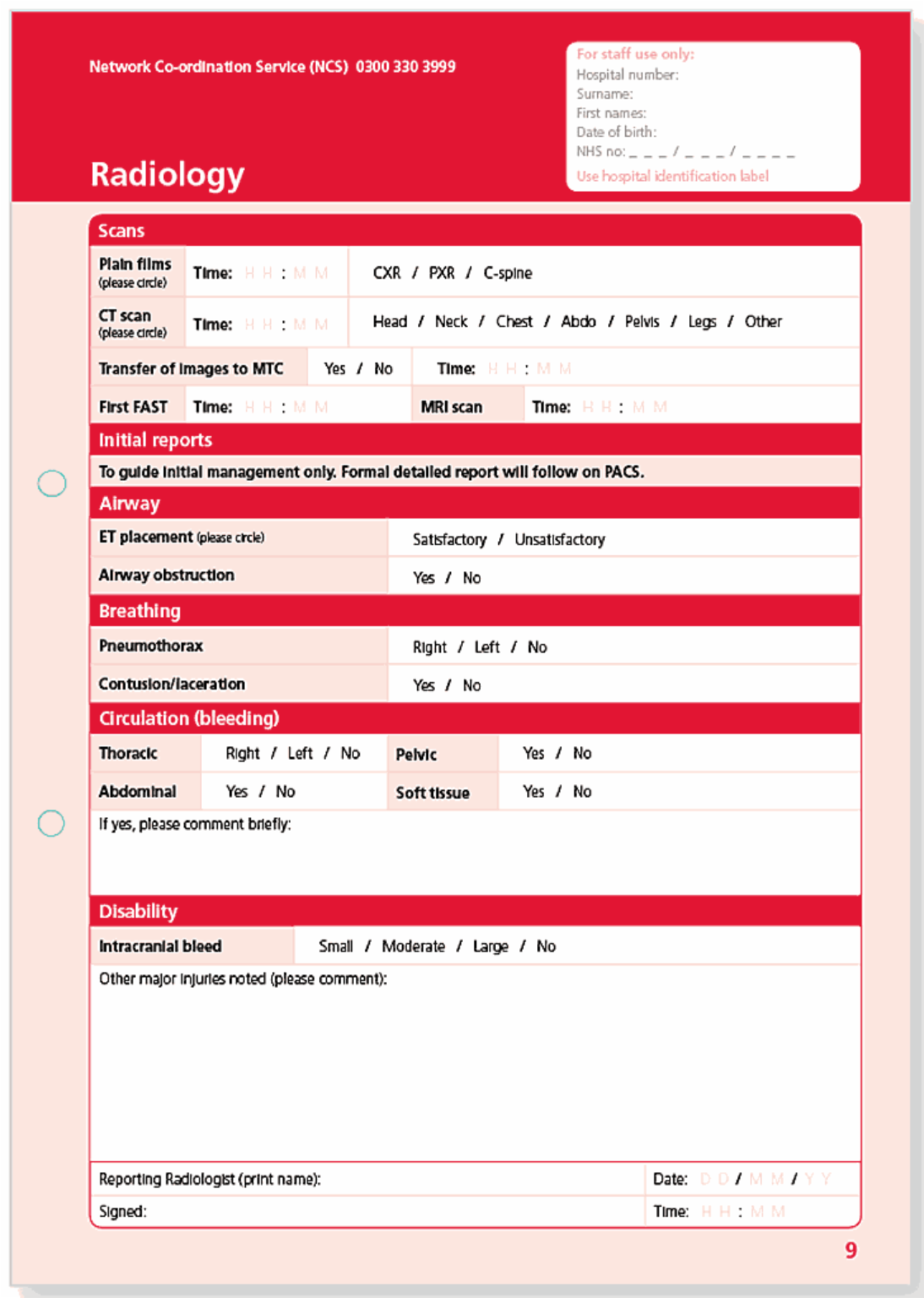
The Emergency department trauma documentation (page 9) provides a means of
reliably communicating immediately life-threatening injuries to the trauma team
and should be completed by the radiologist at the time of the scan. The primary
CT survey / provisional report is not to be used to exclude any injuries.
A formal report should be made available as soon as possible, within an hour
of the end of the trauma CT.
US:
FAST scan should not delay definitive imaging and should only be performed by an accredited practitioner.
| 05.e.i • | Emergency radiology – Appendix 1 |
Major Trauma Centre guidelines for CT imaging in adult blunt polytrauma
Patients should attend the department on a trauma board with adequate IV access. Remove unnecessary metal objects from the imaging field.
1. Standard head CT
Unenhanced axial head CT – either angled to orbitomeatal line or if suspected
facial injury, spiral acquisition through brain and facial bones.
Bone reconstructions on thinnest possible with edge enhancement.
2. Cervical spine CT
Image from foramen magnum to T3–4. Sagittal 2mm and coronal 2mm
reconstructions either on the scanner or using PACS workstation.
Following head and neck imaging, if possible the patient’s arms should be placed
above their head, crossed over the lower abdomen or placed on a pillow over
abdomen.
3. Arterial phase – chest and abdomen
Image from C6 to aortic bifurcation post IV contrast medium; trigger over ascending
aorta, 100mls at 4mls/sec. Acquire thin section axial images on a soft tissue
reconstruction.
(If there is known or suspected pelvic injury, continue through the pelvis to below
the pubic symphysis. If imaging chest to pelvis in arterial phase, consider using
150ml IV contrast medium followed by 50ml normal saline.)
4. Portal venous phase – abdomen and pelvis
Image from domes of diaphragm to below symphysis pubis at 70 secs from the start of the contrast medium injection. Acquire thin section axial images on a soft tissue reconstruction algorithm.
5. Delayed phase
The initial images should be reviewed whilst patient on the CT table and delayed
imaging performed through all areas suspicious for active bleeding or where solid
organ injury detected (particularly renal injury).
Image at approximately 5 mins post IV injection, if clinically appropriate.
Reformat – thoracic and lumbar spine in sagittal and coronal planes,
2mm reconstructions on CT scanner or PACS workstation.
Caveats:
- Known or suspected pelvic trauma: arterial phase should extend to the pubic symphysis.
- If bladder rupture is suspected, CT cystogram should be performed if there is a catheter in situ (50mls of contrast in 450mls of normal saline – bladder filled under gravity – approximately 250–400mls).
- Consider leg run-off in lower limb trauma with clinically suspected vascular compromise (if imaging the lower leg, may need to consider increasing IV contrast medium to 200mls and 100mls normal saline to improve bolus quality).
| 05.e.i • | Emergency radiology – Appendix 2 |
Major Trauma Centre guidelines for CT imaging in paediatric blunt polytrauma
CT is the imaging modality of choice
No pre-contrast imaging of the chest or abdomen
Protocol:
Head / C-spine – if indicated pre IV contrast medium
Chest – single arterial post IV contrast medium, in inspiration if possible
Abdomen/Pelvis – single portal venous phase only
Consider delayed topogram / CT at 10 minutes if urinary tract injury
If bladder injury or pelvic fracture, consider formal cystogram
Oral contrast medium:
A single dose of dilute gastrograffin 10–15 minutes before the examination can be
considered if the patient is clinically able to tolerate this. If the patient is intubated,
this can be given via NG tube following discussion with the anaesthetist.
Scan delay times will vary according to local protocols.
Intravenous contrast medium:
Local protocols must be followed
Within Cambridge University Hospitals Major Trauma Centre:
2mg/kg of warmed Iomeron 300 used, to a maximum of 100ml. Minimum of 10ml
overall volume. If less than 10ml, a saline bolus can be given to make up to 10ml.
The delay from time of injection to imaging will differ between different scanners.
| Age | Dose and dilution |
| 0–1 years | 1ml Gastrografin / 60mls water |
| 2–5 years | 2mls Gastrografin / 125mls water |
| 6–12 years | 3mls Gastrografin / 175mls water |
| 13+ years | 4mls Gastrografin / 250mls water |
| 05.e.i • | Emergency radiology – Appendix 3 |
Penetrating trauma CT protocol
1. Standard head CT – if involved
Unenhanced axial head CT – either angled to orbitomeatal line or if suspected
facial injury, spiral acquisition through brain and facial bones.
Bone reconstructions on thinnest possible with edge enhancement.
2. Cervical spine CT
Image from foramen magnum to T3–4. Sagittal 2mm and coronal
2mm reconstructions either on the scanner or using PACS workstation.
Following head and neck imaging, if possible the patient’s arms should be placed
above their head, crossed over the lower abdomen or placed on a pillow over
the abdomen.
3. Arterial phase – chest and abdomen
Image from C6 to aortic bifurcation post IV contrast medium; trigger over ascending aorta, 100mls @ 4mls/sec. Acquire thin section axial images on a soft tissue reconstruction.
Consider also imaging the neck in the arterial phase, following IV contrast medium, to assess vascular injury secondary to penetrating injury.
4. Portal venous phase – abdomen and pelvis
Image from domes of diaphragm to below symphysis pubis at 70 secs from the start of the contrast medium injection. Acquire thin section axial images on a soft tissue reconstruction algorithm.
5. Delayed phase
The initial images should be reviewed whilst patient is on the CT table and delayed
imaging performed through all areas suspicious for active bleeding or where solid
organ injury is detected or suspected (particularly renal injury).
Image at approximately 5 mins post iv injection, if clinically appropriate.
Oral / rectal contrast medium:
In suspected penetrating trauma to the abdominal or pelvic cavity, rectal and oral
contrast medium can be helpful in the detection of bowel injury.
Oral contrast medium – dilute oral contrast medium can be administered orally
or via NG tube.
Rectal contrast medium – give 1000ml of diluted iodinated contrast medium
delivered via a drip system with a ballooned Foley catheter inserted within
the rectum.
If bladder injury is suspected, CT cystogram or formal cystogram can be undertaken.
If there is a bladder catheter in situ – fill bladder under gravity with 50mls of contrast
medium in 450mls of normal saline.
References
- Standards of practice and guidance for trauma radiology in severely injured patients, (The Royal College of Radiologists, 2011)
- Smith CM, Woolrich- Burt L, Wellings R, Costa ML, ‘Major trauma CT scanning: the experience of a regional trauma centre in the UK’, Emerg Med J (2011); 28: 378–382