Step 1
The primary objective is to concurrently manage hypoxia, tension pneumothorax and hypovolaemia – described as ‘oxygenate, decompress and fill’:
- Oxygenate – endotracheal intubation + ventilation with 100% oxygen
- Decompress – bilateral finger thoracostomies
- Fill – high volume intravascular filling (≥2000ml of crystalloid / blood products)
Activate massive blood loss protocol
→ Section 6.b.iv
Massive blood loss protocol
Step 2
Once the secondary objectives have been commenced, control ongoing haemorrhage:
- Check / apply combat application tourniquets
- Check / apply pelvic binder
- Control haemorrhage:
-straighten long bone deformities
-apply pressure bandages / haemostatic dressings
-address MAXFAX injury
→ Section 6.b.ii
Use of tourniquets
Step 3
Once the secondary objectives have been commenced, consider further interventions:
- Resuscitative thoracotomy
- Resuscitative hysterotomy
- Chest compressions
Early communication with NCS will facilitate activation of additional resources and expertise.
Resuscitative thoracotomy (RT)
RT in penetrating TCA (in order to relieve a cardiac tamponade) is a well-proven
lifesaving intervention and should be undertaken in Step 1 if chest decompression
has not resulted in a return of spontaneous circulation (ROSC). RT may be successful
up to 15 minutes after arrest, but earlier intervention is associated with better
outcomes.
RT in blunt TCA (in order to manually compress the thoracic descending aorta) is not
a well-proven lifesaving intervention, but should be considered by senior providers in
Step 3 if other measures have not resulted in a ROSC. The group of patients who are
most likely to benefit are those in pulseless electrical activity secondary to isolated
haemorrhagic injury to the abdomen and or pelvis.
→ Section 6.a.ii
Resuscitative thoracotomy
Resuscitative hysterotomy (RH)
Females with a gravid uterus palpable above the umbilicus (≥20 weeks gestation) may benefit from RH in TCA. This intervention can be successful up to 15 minutes after arrest, but earlier intervention is associated with better outcomes. Additional teams from obstetrics / gynaecology and neonatology / paediatrics should be alerted to assist subsequent management, but RH should not be delayed until their arrival.
→ Section 6.i
Obstetric trauma
Chest compressions
TCA is fundamentally different to medical cardiac arrest with different causes and underlying pathophysiology. Chest compressions are of little value in TCA and are potentially detrimental to achieving ROSC by delaying the primary objective of ‘oxygenate, decompress and fill’. Once other interventions have been completed (Step 1 & 2) chest compressions may be considered as a method to provide some blood flow to vital organs.
Return of spontaneous circulation (ROSC)
ROSC in TCA is defined as the presence of a palpable central pulse. These patients should be considered as ‘peri-arrest’, and the following actions undertaken:
- Review Steps 1, 2 & 3
- Aliquots of warmed crystalloid / balanced blood products to maintain a central pulse. If traumatic brain injury is considered to be the dominant condition use a less restrictive fluid resuscitation approach. Invasive blood pressure monitoring will improve awareness of the patient’s cardiovascular status.
- Plan for immediate definitive haemorrhage control (damage control surgery +/- interventional radiology)
- Sedation and paralysis as indicated
- Pre-hospital teams should alert the receiving hospital and specifically request activation of the major haemorrhage protocol and a senior surgical team.
Terminating resuscitation
After 20 minutes (and completion of Steps 1, 2 & 3) without a ROSC, termination of resuscitation efforts should be discussed with the team. Asystole, failure to respond to Steps 1, 2 & 3 interventions, and external brain matter are all associated with a poor outcome. Organ donation may be considered after a decisions is made to terminate resuscitation.
→ Section 6.j
End of life care
Team factors
TCA should be aggressively managed using a standardised approach that rapidly addresses reversible causes in order of priority. To achieve this providers must be familiar with the Step 1, 2, 3 principle and team roles allocated below.
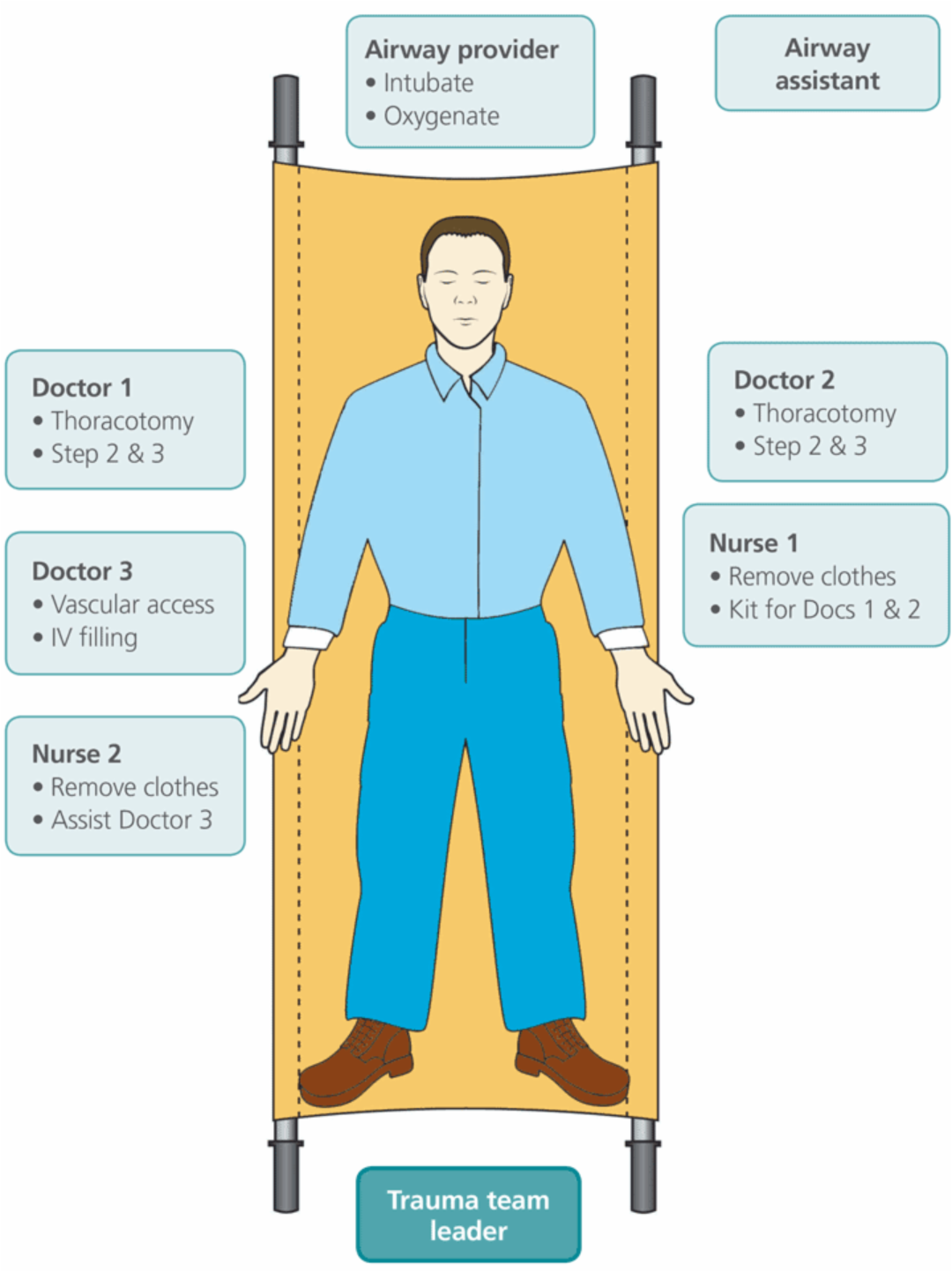
It is recognised that pre-hospital teams will make best use of available personnel to achieve the TCA objectives in the same priority order as in-hospital teams.
Follow-up
TCA is a rare and stressful event – extra attention should be paid to clinical and personal debriefing.
→ Section 5.g
Trauma team debrief