Clinical context
There are over 8,000 people waiting for an organ transplant in the UK.
The identification of potential donors in emergency departments (ED) will increase
rates of donation and will ensure patients’ previously held wishes are fulfilled.
It has been suggested that the overall incidence of brain stem death in the UK may
be falling because patients with catastrophic brain injury are not admitted to critical
care and have treatment withdrawn in the ED, meaning formal brain stem death
testing is not carried out.
The potential for donation within the ED mainly comes from severely brain injured
patients; either from trauma or acute medical catastrophe, eg. sub-arachnoid
haemorrhage, or in patients who are post cardiac arrest with return of spontaneous
circulation (ROSC).
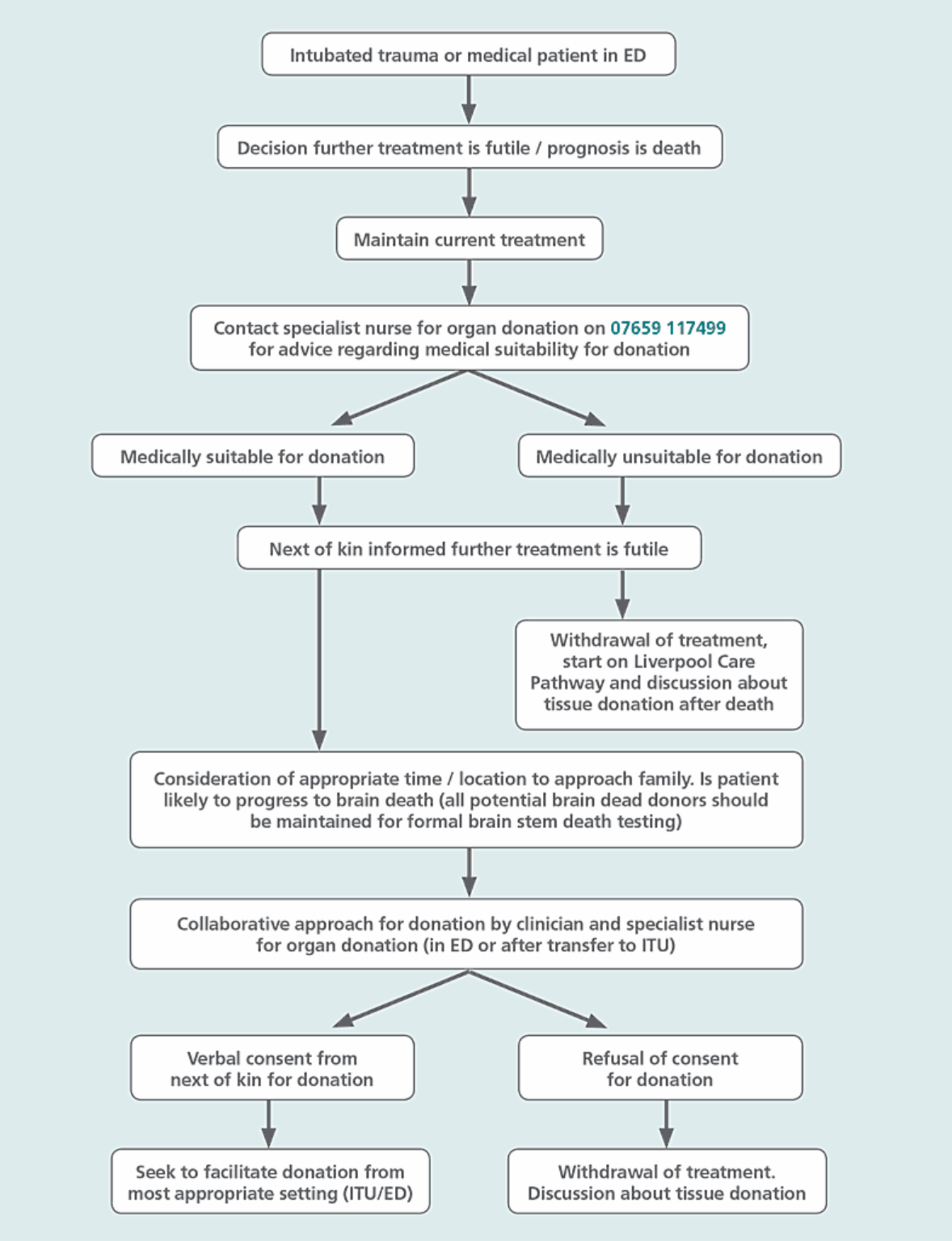
Best practice
This pathway has been written to advise and guide senior members of ED staff
in decision-making around organ donation.
Where a ventilated patient has suffered a catastrophic traumatic or medical event,
and the decision has been made that further treatment is futile, a specialist nurse
for organ donation (SNOD) should be contacted as the next step.
When the decision has been made that further treatment is futile, it is essential to
continue to care for patients in a critical care environment while donation is being
considered / explored.
It is important to consider if the patient is likely to progress to brain stem death.
Donation via brain stem death results in a greater number of donated organs. The
Academy of Medical Colleges and the Intensive Care Society state that best practice
is to undergo formal brain stem death testing where brain stem death is likely but
irrespective of organ donation. Please seek the advice of your consultant intensivist.
Unless raised by the family, the issue of donation should not be discussed until the
decision to withdraw life-sustaining treatment has been understood by the family.
It is best practice to ‘decouple’ conversations regarding patient prognosis, treatment
futility and death with conversations exploring organ donation, ensuring these two
distinct clinical conversations are had at separate times.
When a decision has been made to approach families about organ donation best
evidence suggests that a collaborative approach with a senior clinician and a SNOD
should be undertaken.
Facilitating donation takes many hours and agreed local policies should guide where
the most appropriate environment is to care for these patients (ICU, ED or other
capable areas such as theatres / recovery). An agreed local policy should suggest
potential alternative areas and staffing.
Patients who die in the ED
Patients in whom further treatment is futile, and who are dying, should routinely
be started on the Liverpool Care Pathway.
Patients who die in the ED from any cause may be suitable eye and tissue donors.
The next of kin should be offered this routinely and, if they consent, tissue services
should be contacted on 0800 432 0559. They can offer advice and will contact the
family to answer questions and go through the formal consenting process. Eyes and
tissues for donation can be retrieved up to 24 hours after death.