Penetrating cardiac injury has two main modes of presentation:
- cardiac tamponade
- hypovolaemia
A patient may display features of both tamponade and hypovolaemia.
When a penetrating cardiac injury in a child is suspected:
- Paediatric Trauma Call with early alerting of:
- NCS
- Emergency Department Consultant
- Anaesthetic Consultant on-call
- Consultant Paediatric Surgeon on-call
- Theatre Co-ordinator
- Trauma team must ensure that an emergency thoracotomy set is available in the resuscitation room.
- An emergent thoracotomy (in ED or in theatres) should be performed if the patient:
- arrests in ED / Theatres
- is peri-arrest
- arrested within 10 minutes of arriving in ED.
- The decision to perform a thoracotomy should be made by the trauma team leader.
Emergency thoracotomy
Emergent thoracotomy is used to gain rapid access to the thoracic cavity to facilitate immediate intervention in resuscitation. It is sometimes referred to as resuscitative thoracotomy.
Emergent thoracotomy is often aimed solely at managing those patients with a simple cardiac wound leading to tamponade and cardiac arrest.
Indications for emergent thoracotomy
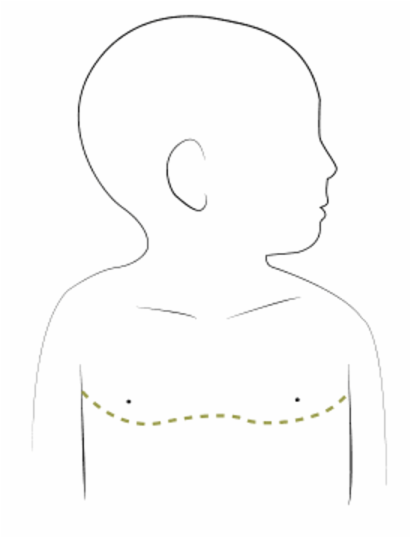
Penetrating injury to the anterior box resulting in:
- cardiac arrest that has occurred within 10 minutes
- effective BLS has been delivered in the period from start of cardiac arrest until the decision to perform the thoracotomy is made.
Contraindications for emergent thoracotomy
Absolute
- No signs of life (or CPR) for >10 minutes.
Relative
- Gunshot wounds
- Blunt injuries
Technique
Instruments:
- Skin marker
- Skin prep
- Scalpel
- Sterile scissors (eg. Mayos or Tuff-Cuts)
- Appropriately sized clips
- Gigli saw
- needle holder
- Forceps - DeBakeys
- Suction
- Foley catheter
Procedure:
Thoracotomy
- Patient should be intubated and ventilated and have good venous access. This can be done simultaneously as performing the thoracotomy by other members of the team.
- Abduct both arms to 90 degrees.
- Mark sites for thoracostomies bilaterally and skin incision (following 4th or 5th ICS, and joining up in midline) with a skin marker.
- Gown and glove.
- Prep skin with chlorhexidine or betadine.
- Create bilateral thoracostomies.
- If the patient has a ROSC after thoracostomies do not proceed to thoracotomy.
- Create long skin incision joining thoracostomies along line that was marked.
- The incision should extend from right posterior axillary line to left posterior axillary line. Failure to take the incision far enough posteriorly will result is difficulty opening the chest.
- This first incision should extend through skin, to subcutaneous fat.
- Using a large pair of sterile scissors, extend the thoracostomies to the sternum. Guard against injury to underlying lung and heart during this step.
- Use the scissors to cut the sternum.
- If the sternum cannot be cut using scissors pass a suitable clip behind the sternum and pass through Gigli saw. Attach the saw blade to handles and saw through the sternum (should not take more than 2–3 pulls).
- Lift the anterior chest open. Get an assistant to hold the chest open.
- Divide the fibrofatty tissue (thymus or remnants) as close to sternum as possible.
- If there is difficulty in lifting the chest high enough, consider extending the incisions posteriorly.
Open pericardium
- Identify the heart. If a tamponade is present, the pericardium will appear tense, dark and bulging.
- Apply two clips to pericardium on anterior surface, tent up and open pericardium between clips.
- If you go too high the pericardium will be thicker and more difficult to mobilise.
- Keeping anterior will avoid damage to phrenic nerve, which runs along left lateral border of the heart.
- Divide the pericardium superiorly and inferiorly with scissors.
- Evacuate clot from pericardium using your hands and inspect heart.
Bi-manual cardiac massage
- If the heart makes no spontaneous movement start internal cardiac massage.
- Place right hand behind heart.
- Place left hand over anterior surface of heart with apex lying against palm.
- Squeeze heart from heel of hand towards fingers in a milking motion.
- Keep hands flat.
- Avoid direct pressure with the finger tips into heart muscle as this may cause myocardial rupture.
Cardiac wounds
- Identify any cardiac lacerations.
- Small wound (< 1 cm) can be left if there is little blood loss.
- If a cardiac laceration bleeds significantly the options are:
- Use pericardial buttresses to prevent the suture tearing through the myocardium.
- Place the first sutures at the lateral edges of the laceration to prevent it from extending.
- Be careful of occluding coronary arteries when placing sutures.
- Be careful not to plug the hole with a finger as this may simply extend the wound.
- Do not over inflate balloon of Foley catheter as this may impair ventricular filling.
- Do not pull too hard on the Foley catheter as this may cause it to tear through the myocardium, leading to a much larger myocardial tear.
- Counter traction should be applied to the Foley catheter to stop it pulling through the myocardium.
- Ensure that you check the posterior surface of the heart. This can be achieved by gently lifting it up. Be aware that if you lift the heart too much you can occlude the great vessels.
To suture wound:
Occlude wound with finger
Occlude wound by inserting a Foley catheter and inflating balloon
Pulmonary wounds
- If there is an obvious bleeding pulmonary wound it should be sutured.
- For unilateral pulmonary injury with extensive blood loss, and no obvious wound
this may be controlled immediately by:
Clamping the hilum with a Satinsky clamp
Performing a pulmonary hilar twist2
- Divide inferior pulmonary ligament – there is a small vein immediately below the ligament which acts as a useful landmark.
- Lower lobe is then rotated anteriorly over the upper lobe (twists vessels around bronchus).
- Maintain position by packing chest.
- This results in physiology similar to that seen during pneumonectomy.
Hypovolaemia
- If hypovolaemia turns out to be the primary pathology then the following manoeuvres can be considered:
- Clamp aorta as low as is possible. This can be achieved by digital pressure to buy time for dissection to allow an aortic cross clamp to be applied.
- If a Foley catheter has been used to occlude a cardiac laceration this can be used as a route for administering WARM fluids.
- Fluids given directly into the heart must be warm to avoid the risk of cardioplegia.
Ventricular fibrillation
- Should this occur, close chest.
- Apply defibrillator pads to chest wall as normal and defibrillate.
- Ensure that there are no pools of fluid that may cause arcing.
Return of spontaneous circulation (ROSC)
- Following ROSC there will be bleeding from the inferior mammary arteries. This should be controlled by clipping or ligating these vessels.
- If the patient is in theatre all identified injuries should be addressed as clinically appropriate.
- If the patient is in the ED they should be anaesthetised as required and transferred to theatre for completion of the thoracotomy.