Blunt abdominal trauma
Blunt abdominal trauma in children tends to be managed in a much more conservative manner than in adults. Children are abdominal breathers. Therefore, any abdominal injury will compromise the ventilatory effort of children. The task of initiating interventions, which improve ventilation in these patients, is as important to the managing clinician as making decisions regarding the management of the intra-abdominal injury.
General algorithm for managing blunt abdominal trauma in a child
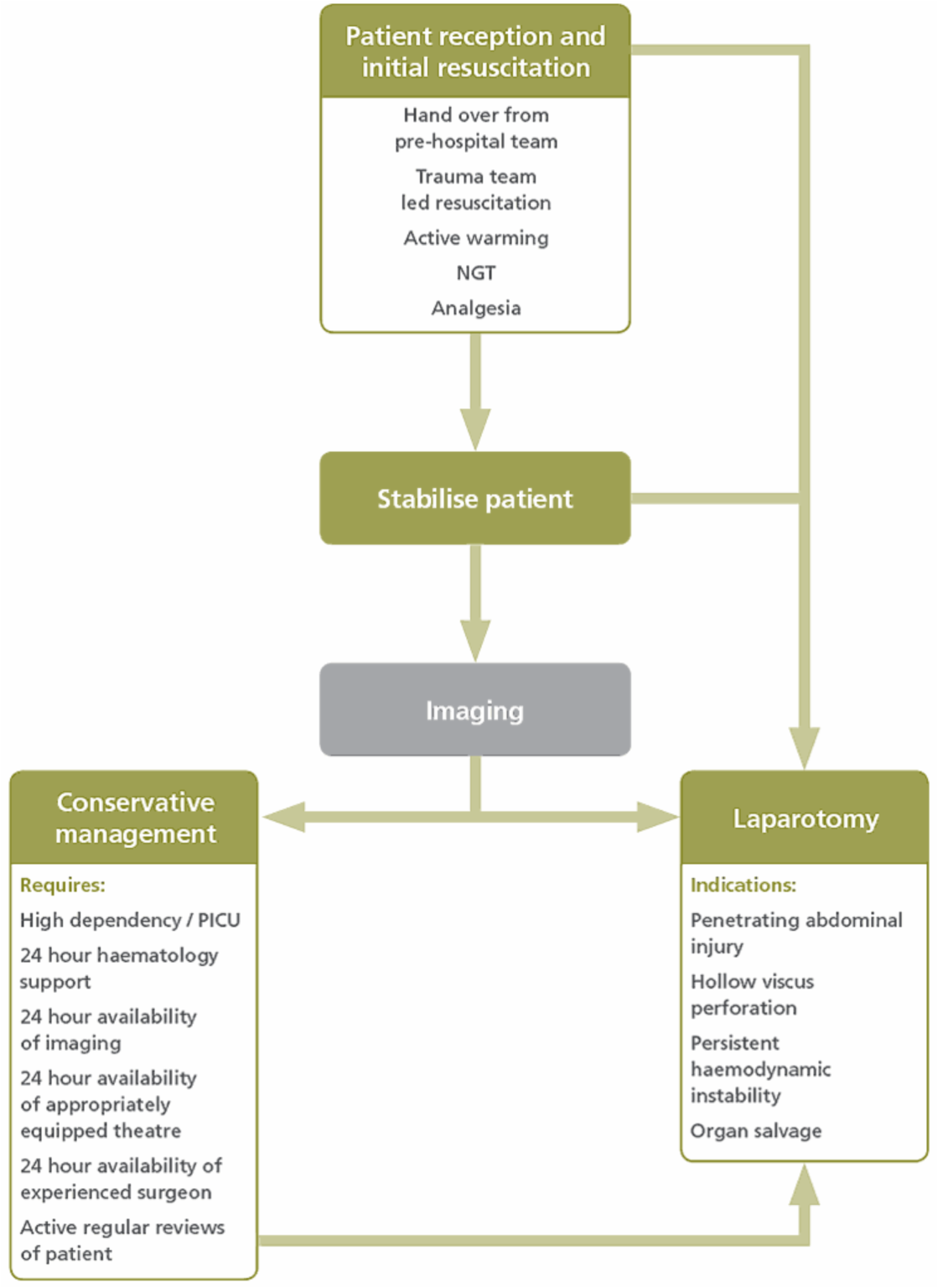
Considerations in ED resus:
- Ensure blood is available early in the resuscitation. The paediatric massive blood loss protocol should be initiated as soon as the presence of significant blunt abdominal trauma is recognised.
- Place a nasogastric tube in all children with blunt abdominal trauma if no head injury. All children with suspected intra-abdominal injury should receive antibiotics (due to the risk of hollow viscus perforation). All children should receive adequate analgesia at an early stage. This will help their breathing as well as being humanitarian.
- Hypotensive resuscitation has no place in the management of children with blunt abdominal trauma; a child possesses a large physiological reserve, and so hypotension is a preterminal sign.
- All trauma patients should have a urinalysis.
- Initial imaging
The gold standard imaging modality for children with blunt abdominal trauma is CT scan with contrast. Only CT imaging can give accurate information regarding grading of injury to solid intra-abdominal organs. - Decisions regarding conservative management should be based on:
- the haemodynamic status of the child
- results of CT imaging.
- Discuss the patient early with a paediatric surgeon for all management decisions and the best place for patient’s management.
- Monitoring
Record observations every 15 minutes for the first 4 hours of admission, and then every 30 minutes for the first 12 hours. They should then be recorded hourly until the first 24 hours is complete.
Fluid balance should be closely monitored so that an accurate picture is obtained. - For conservative management:
- two routes of vascular access should be obtained
- bloods for cross-matching, full blood count and coagulation studies
- fluid resuscitate patient using 10ml/kg boluses of warm fluids (after 40mls/kg crystalloid has been given since injury blood should be used)
- correct hypothermia and coagulopathy if present.
- strict bed rest.
The decision that conservative management has failed and that the patient requires
a laparotomy rests solely with the responsible surgeon.
Always consider if interventional radiology may be an alternative to laparotomy.
Penetrating abdominal trauma
As a general rule all penetrating wounds require exploration.
General algorithm for managing penetrating abdominal trauma in a child
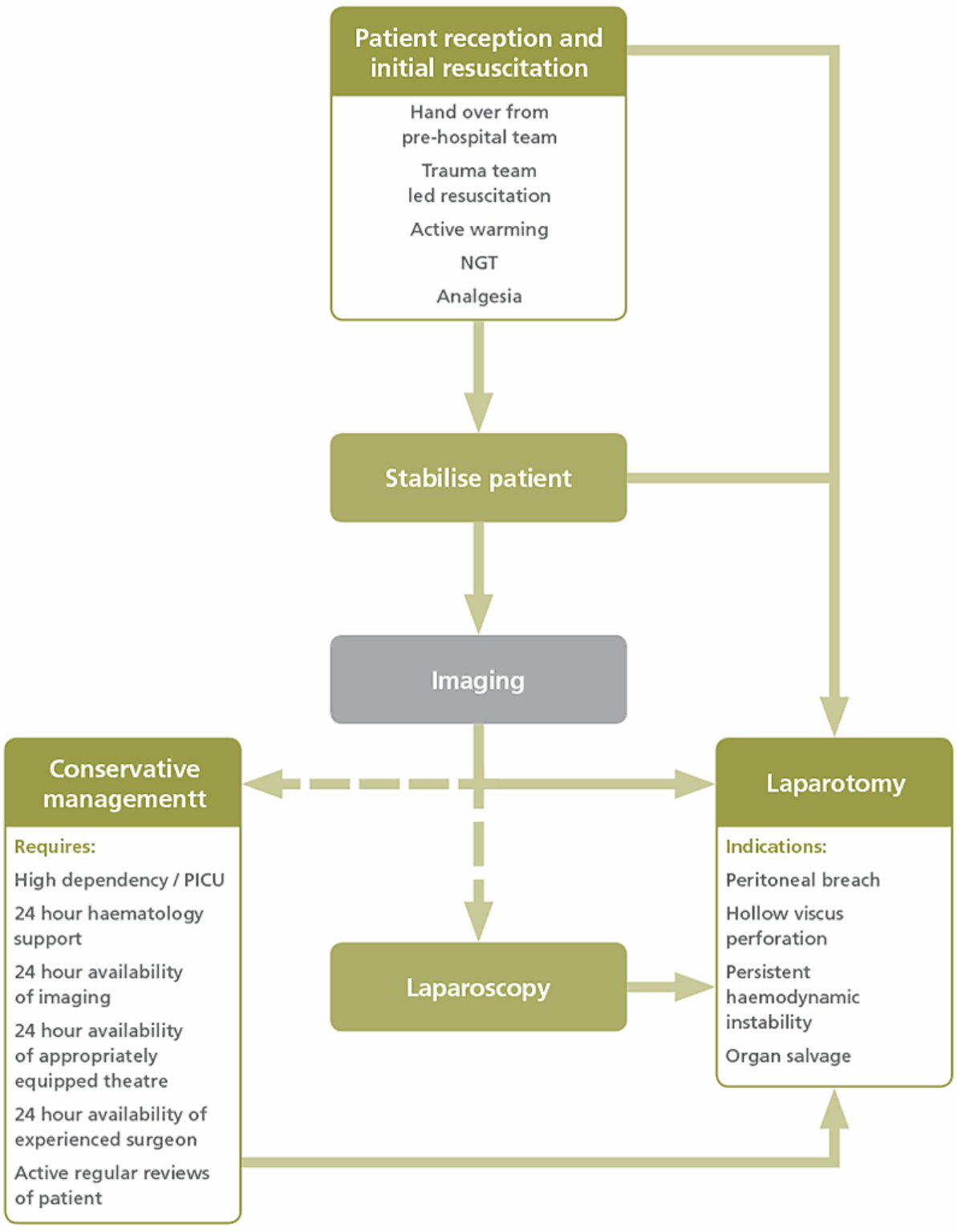
- Paediatric massive blood loss protocol should be activated early.
- If the patient is stable imaging (CT scan with IV contrast) should be performed to gain more information regarding the exact nature of the injury.
- There is significant risk of major vessel injury.
- If a foreign body is still in place, it should not be removed in the emergency department. It should only be removed in a theatre, which is fully equipped and staffed. When the foreign body is being removed, the surgeon must be prepared to perform an emergency laparotomy to gain vascular control if the patient deteriorates rapidly.
- Penetrating trauma may involve more than one region:
- stab wounds of the lower intercostal spaces may involve the chest and the abdomen
- stab wounds of the anterior box (see section 7.c.vi) may traverse the peritoneum to penetrate the heart.
- If there are clear signs of peritoneal breach (free air on imaging, peritonism, abdominal distension) urgent laparotomy should be performed. Ideally this should be performed by a paediatric surgeon. If the patient is too unstable for transfer the case should be discussed with a paediatric surgeon. If there is doubt regarding peritoneal breach, the wound should be explored under general anaesthetic, with the surgeon able to proceed and deal with findings. Exploration under local anaesthetic is rarely satisfactory.
→ Section 7.c.vi
Penetrating thoracic trauma