A patient who has sustained a spinal cord injury (SCI) will have anaesthetic skin
below the level of their injury, therefore development of severe pressure ulcers can
occur quickly as the person would have no awareness that a problem is developing.
The most common sign that a pressure sore is beginning is the appearance of
a red area, or red spot on the skin. Ordinarily, redness should clear within 30 minutes
after the pressure is released from the area. If the redness does not clear, a pressure
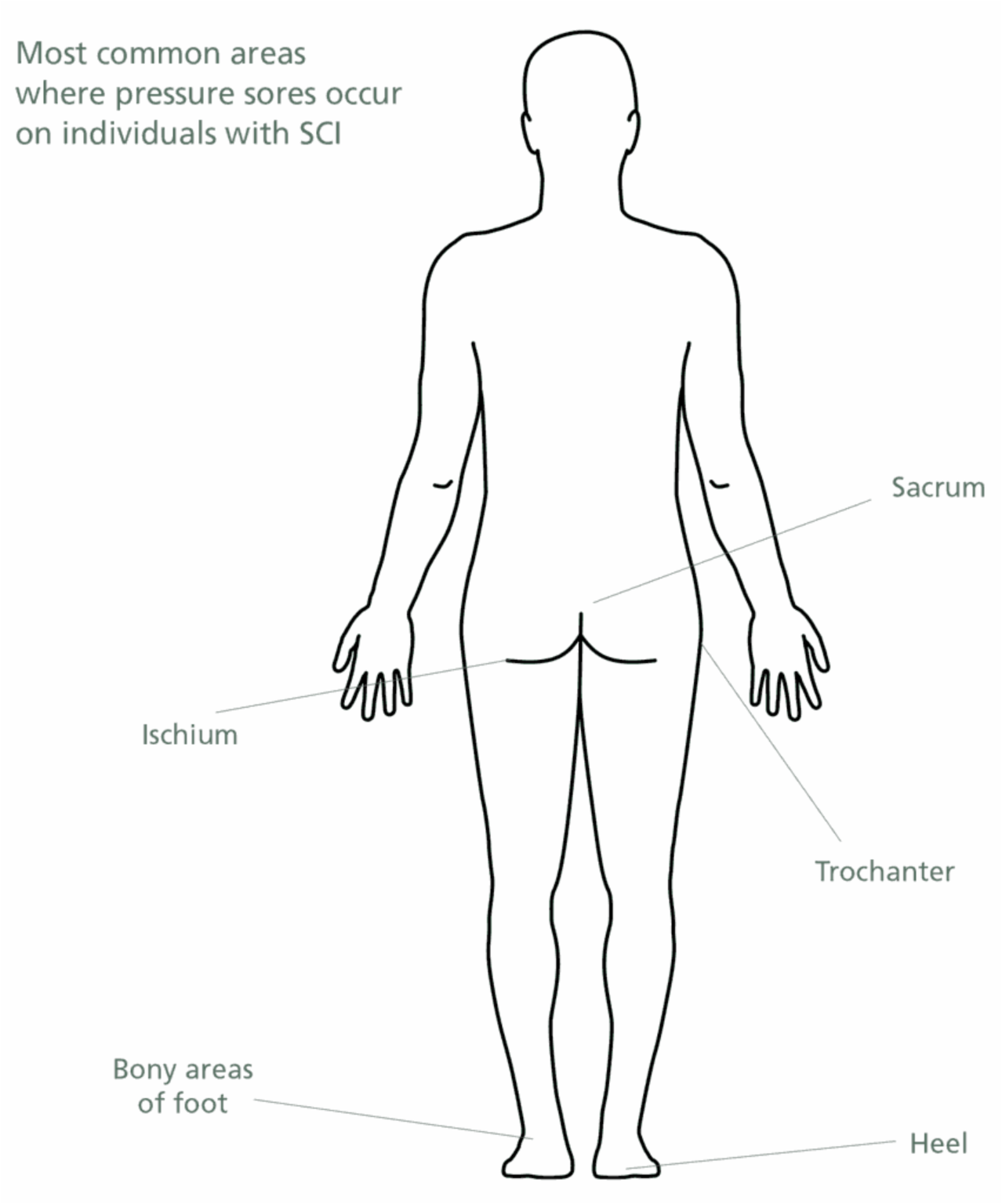
sore has begun. Non-use of muscles around the bony prominences of the body (hips,
heels and elbows, sacrum and ischium) leads to muscle loss (atrophy), adding to the
risk of skin breakdown. Any skin breakdown would mean that even once healed,
the area would remain vulnerable to further breakdown in the future.
- The force of friction or shearing (the dragging movement of skin tissues across a surface), such as sliding in a bed or chair can cause blood vessels to stretch or bend, leading to pressure ulcers.
- An abrasion can occur when pulling across a surface instead of lifting.
- A bump or fall may cause damage to the skin that may not show up right away.
- People with limited sensation are also prone to skin injuries from burns.
Pressure sores can be caused by clothing, braces, or hard objects that put pressure on the skin. For example, following removal of any splint, skin will need to be checked thoroughly for any abrasions or marks to the skin to reduce the risk of skin deterioration.
Clinical management guidelines
For pressure sore prevention:
- Record the patient’s Waterlow score and MUST score on admission and monitor these weekly.
- Ensure that the correct mattress is used on the bed, and the correct cushion if a wheelchair is used – this is guided by the Waterlow Score.
- The Patient’s skin needs to be checked for pink/red marks or abrasions prior to them getting dressed each morning and again on their return to bed.
- Encourage or assist the patient to relieve pressure whilst sitting up in wheelchair for 2 minutes every hour.
- Keep the patient’s skin clean and dry. Wet skin can become soft, inflamed and is less resistant to damage – wash and dry skin right away after any bowel or bladder accident; change clothes if they become wet.
- Use lotion instead of powder on skin.
- Encourage the patient to eat a well-balanced diet. Foods high in protein, vitamins and minerals help skin stay healthy and heal more quickly.
- Refer the patient to the dietician if indicated by the MUST score.
- Encourage to patient to drink – drinking the recommended amount of fluids to help skin stay soft.
For management if a pressure area develops:
- The key action on noticing a pressure mark on the skin is to remove pressure from the area.
Dependant on the location of the mark, this may necessitate a period of bed rest. However if an ulcer develops it could take months to heal, and many people with spinal cord injuries are hospitalised for lengthy periods due to skin breakdown.
- Involve the Tissue Viability Nurse Specialist for advice on treatment or dressing of the area.
- It is essential to follow a rigorous, rigid turning regime.
- Reassess Waterlow and upgrade pressure relieving equipment as indicated.
- Reassess MUST score and refer to dietician (if not previously indicated by MUST score).
References
Pressure Ulcer Risk Assessment and Prevention (NICE, 2001)
European Pressure Ulcer Advisory Panel (EPUAP), Pressure Ulcer Prevention and Treatment Guidelines (1998), www.epuap.org