The technical definition is ‘velocity-dependent increased resistance to passive limb
movement in people with upper motor neurone syndrome’ (Lance 1980).
At a clinical level, there are two main contributing factors to resistance to movement
in the context of limb spasticity following damage to the brain or spinal cord:
- neurogenic component: overactive muscle contraction
- biomechanical component: stiffening and shortening of the muscle and other soft tissues
Harmful effects of spasticity include:
- pain
- difficulty with seating and posture
- fatigue
- contractures
- pressure sores
- deformity
- distress and low mood
- poor sleep patterns
- reduced function and mobility
- difficulty with self care and hygiene
Spasticity is not always harmful. Patients with a combination of muscle weakness and spasticity may rely on the increased tone to maintain their posture and aid standing or walking.
Clinical management issues to consider
Prevention of aggravating factors:
- pain or discomfort
- constipation
- infection (eg. urinary or respiratory tract infection, pressure sores etc.)
- tight clothing or catheter bags
- poor postural management
24-hour postural management programme
- document range of movement (ROM) of arms and legs (can patient feed self, lay down straight and sit in a chair?)
- consider a ‘tilt in space’ wheelchair if it facilitates early mobilisation
Physical therapy aims
- maintain muscle and soft tissue length across joints
- facilitate care giving (passive functional improvements)
- facilitate active control of any residual movements to allow for active participation in tasks (active functional improvements)
Medical treatment (in conjunction with physical therapy)
- consider whether the spasticity is actually harmful and what impact treatment will have in the patient’s functioning
- consider pattern of spasticity: generalised, focal or multi-focal problems
- quantify spasticity using Modified Ashworth Scale
A management strategy can be a combination. While formulating such strategy, consider:
- the different medications (eg. baclofen, tizanidine, gabapentin) and strategies available and their potential uses. If spasticity is combined with neurogenic pain, consider gabapentin as first choice
- mode of administration (pharmacology) and dosing / technique used
- mechanism of action of treatment(s) chosen
- side effects, precautions and potential complications
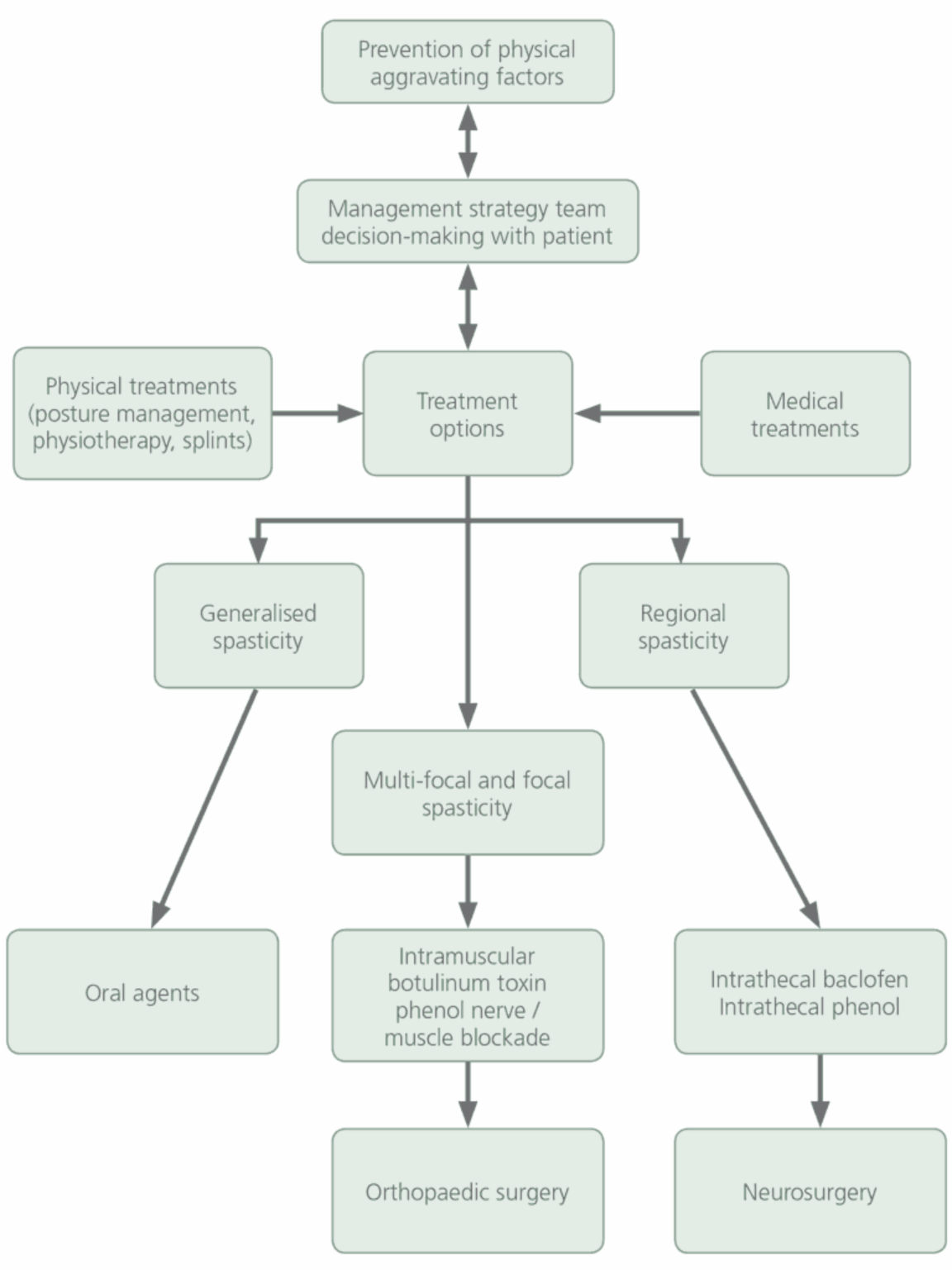
Management strategy for adults with spasticity
(reproduced with permission from Spasticity in adults: management using botulinum toxin, National guidelines, Feb 2009)
References
Spasticity in adults: management using botulinum toxin (National guidelines, February 2009)