Record of amendments
| Amendment no. | Date | Inserted by |
This agreement outlines the protocols and principles for the major
trauma patient flow between the acute trusts in the East of
England Integrated Trauma System.
This major trauma patient flow agreement is between the East of
England Trauma Network Office, acute trusts and commissioning
bodies – named below.
| Major Trauma Centre |
| Cambridge University Hospitals NHS Foundation Trust |
| Trauma units |
| Bedford Hospital NHS Trust |
| Colchester Hospital University NHS Foundation Trust |
| East and North Hertfordshire NHS Trust (Lister Hospital) |
| Ipswich Hospital NHS Trust |
| James Paget University Hospital NHS Foundation Trust |
| Luton and Dunstable Hospital NHS Foundation Trust |
| Mid Essex Hospital Services NHS Trust |
| Norfolk and Norwich University Hospital NHS Foundation Trust |
| Peterborough and Stamford Hospitals NHS Foundation Trust |
| Princess Alexandra Hospital NHS Trust, Harlow |
| Queen Elizabeth Hospital King’s Lynn NHS Trust |
| West Suffolk NHS Foundation Trust |
| Local emergency hospitals |
| Hinchingbrooke Hospital Healthcare NHS Trust |
| Ambulance service |
| East of England Ambulance Service Trust |
| Commissioning |
| NHS England – East Anglia local area team |
| Cambridgeshire and Peterborough CCG |
| North East Essex CCG |
| NHS West Suffolk CCG |
| West Essex CCG |
| Bedfordshire CCG |
| NHS East and North Hertfordshire CCG |
| NHS Great Yarmouth and Waveney CCG |
| NHS Mid Essex CCG |
| North Norfolk CCG |
| West Norfolk CCG |
Contents
|
i.
|
Introduction |
|
ii.
|
Transfer of trauma patient from scene to Major Trauma Centre (MTC) or Trauma Unit (TU)– EoE Major Trauma Triage Tool |
|
iii.
|
Secondary transfer of trauma patients from a TU – call and send protocols |
|
iiii.
|
Reverse transfer of major trauma patients from a MTC back to a local TU – call and receive protocol |
|
v.
|
Summary of responsibilities to ensure effective patient flow |
|
vi.
|
Financial penalties |
|
vii.
|
Incident reporting |
| 12.a • | Introduction |
A recurrent finding in analysis of trauma care is that secondary emergency transfers from emergency departments or inpatient areas to Major Trauma Centres can take a long time to organise – from a personnel, equipment and transport platform perspective. Even when these aspects are addressed a further delay is often created by the need to:
- formally refer the patient to an on-call team
- Transfer images to the receiving hospital. The receiving hospital then has to communicate the acceptance of the transfer. The National Clinical Advisory Group recommended that:
- Networks take the responsibility for the emergency transfer of patients between hospitals in the Network.
- Network co-ordinators should be available 24/7 to manage the transfer of patients.
- MTCs should be capable of accepting immediate transfers without warning.
This agreement seeks to encourage a planned, co-ordinated and timely approach to
the transfer and repatriation of all patients who have suffered traumatic injury across
the East of England (EoE). All trauma patients in the EoE who trigger the Trauma
Triage Tool, will receive care either in nearest Major Trauma Centre (MTC) or the
nearest Trauma Unit (TU), and then transferred if necessary to the MTC or another
TU with specialist services.
This agreement is divided into three parts and covers:
|
Blue light transfer of trauma patients to a MTC or TU, in accordance with the East
of England Trauma Triage Tool, from the scene of the incident. |
|
Secondary transfer of major trauma patients from a TU to the MTC. |
|
Reverse transfer of major trauma patients from a Major Trauma Centre back
to a local Trauma Unit or rehabilitation provider. |
| 12.a.ii • | Transfer of trauma patient from scene to MTC or TU |
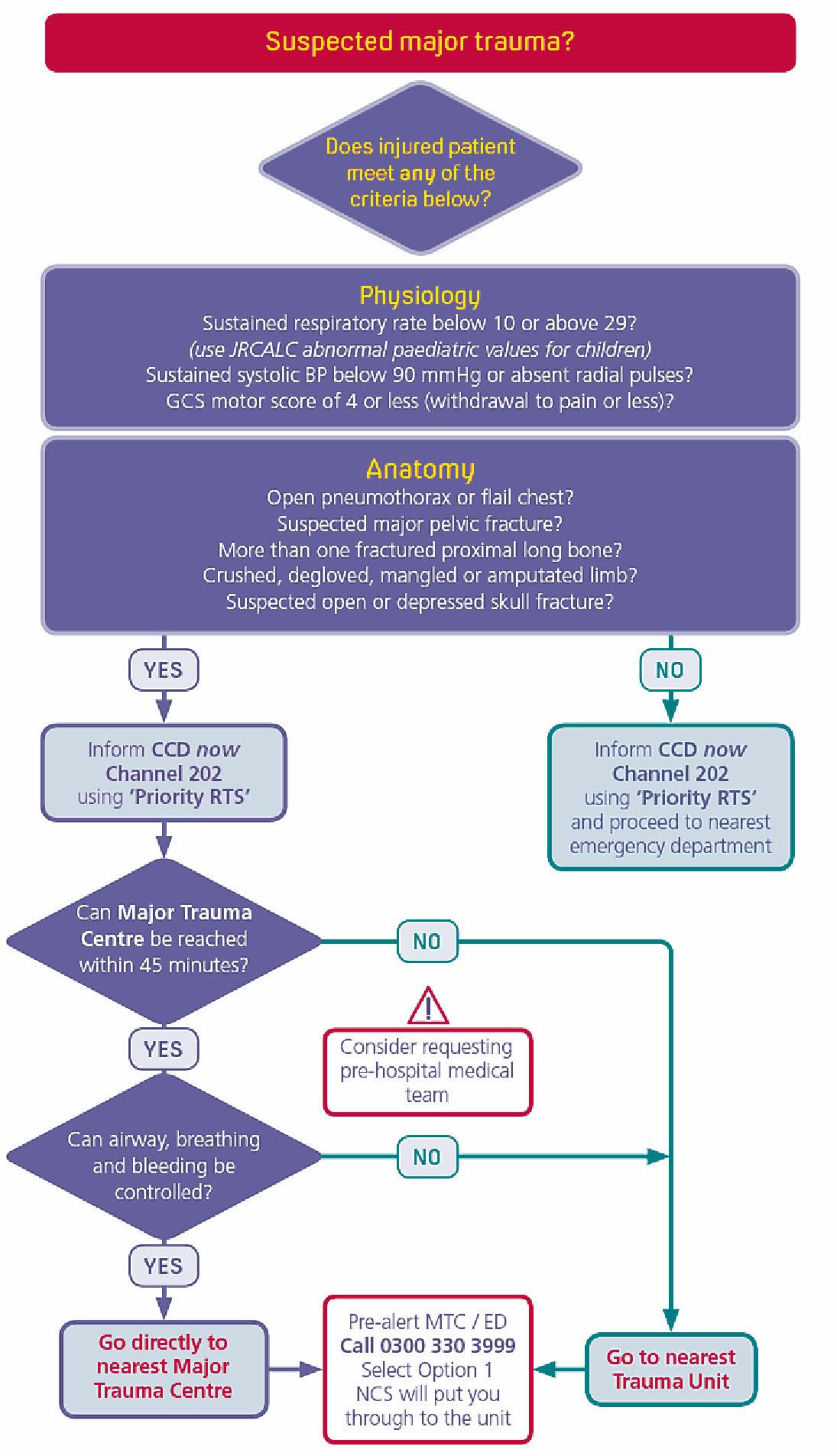
The EoE Major Trauma triage tool is used to determine:
- whether the patient meets the candidate major trauma patient criteria
- the appropriate hospital to transfer to:
- MTC: patient taken to the nearest MTC if within 45mins and possibly bypassing a local ED
- TU: patient taken to the nearest TU if MTC is more than 45mins
NB. In the event of exceptions to the Trauma Triage Tool MTC acceptance must be sought before transfer can take place.
All pre-alerts and handovers should use the ATMISTER system:
Age
Time
Mechanism
Injuries
Signs
Treatment
ETA
Requests
| 12.a.iii • | Secondary emergency transfer of trauma patients from a TU |
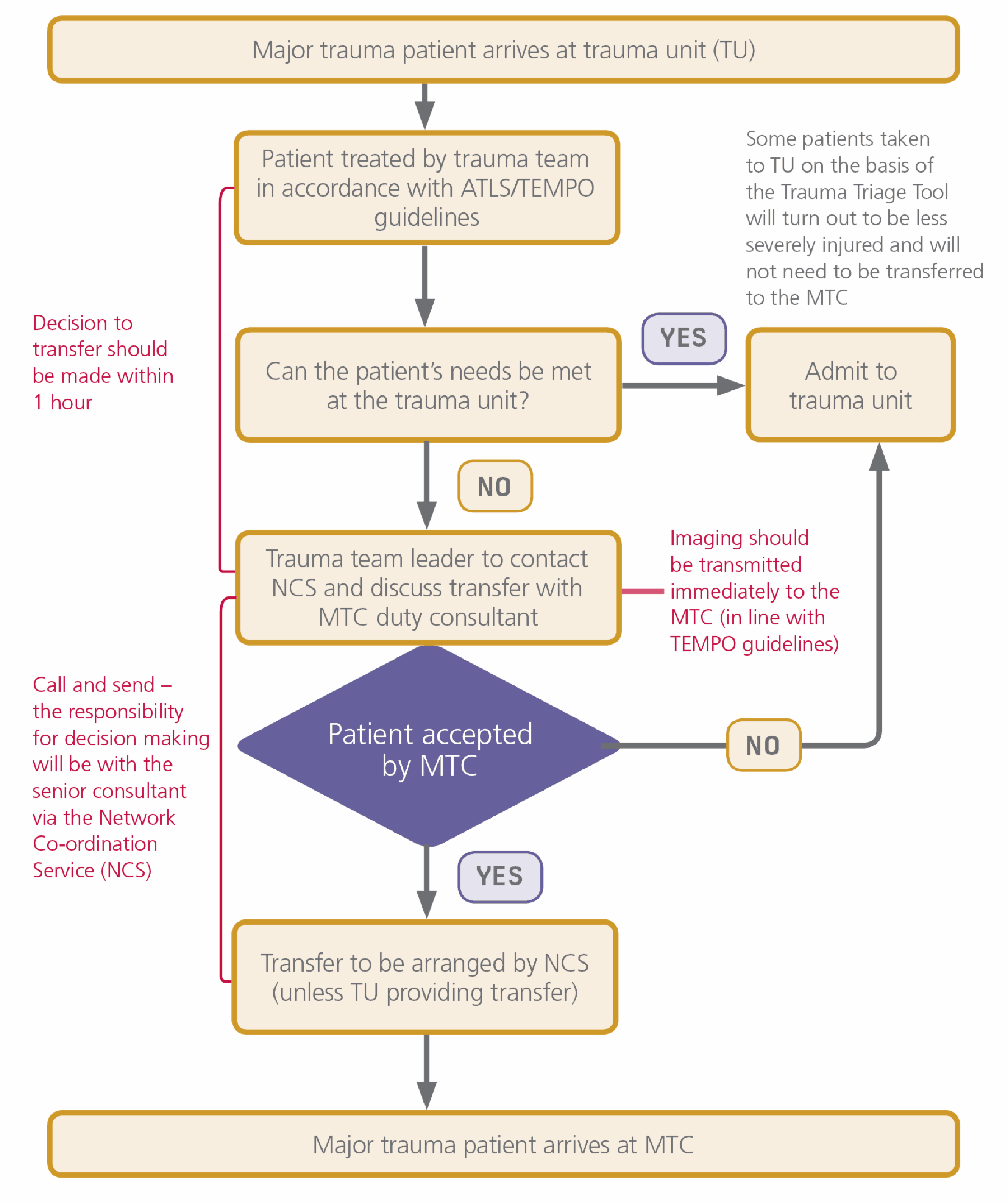
The emergency department communicates the need for secondary emergency
transfer, according to the thresholds and clinical guidelines outlined in the Trauma
East Manual for Procedures and Operations (TEMPO) and then calls to agree the
transfer. The Network Co-ordination Service facilitates the clinical consultation
between the referring ED Trauma Team Leader, the duty MTC Consultant, and where
necessary a Specialty Consultant.
The ‘call and send’ should normally be an immediate transfer from the emergency
department in the TU after resuscitation. Where possible there should be no delay to
the secondary emergency transfer of these patients.
The call and send protocol authorises any emergency department within the network
to commence the process of transferring a patient.
Call and send protocol A: TU to MTC without waiting for the historical referral–
acceptance process to be complete.
Call and send protocol B: TU to a TU with specialties services or a specialist centre
1. The following protocol should be used for call and send to the MTC.
2. The following protocol should be used for ‘call and send’to a TU specialist services or a specialist sentre:
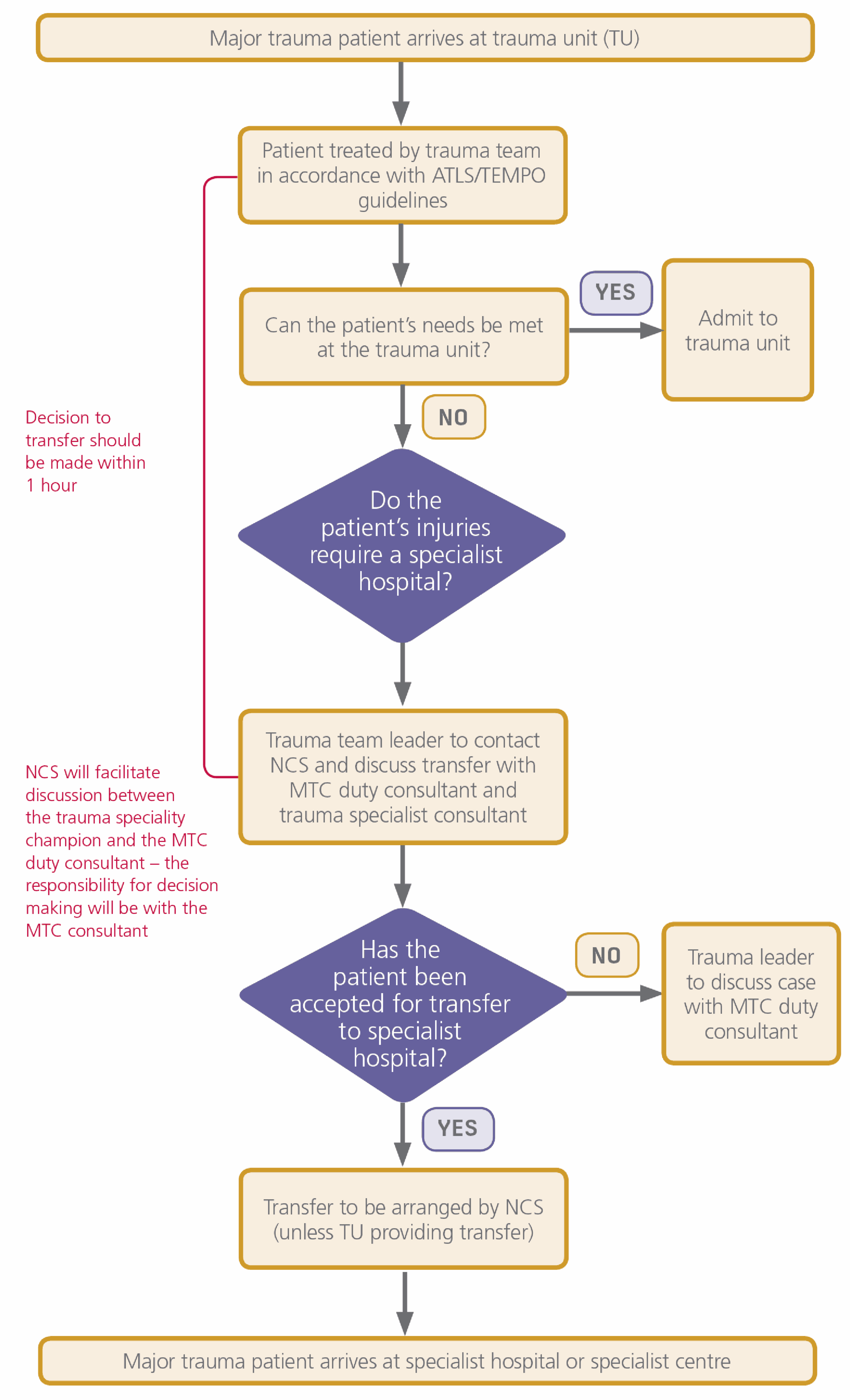
Network Co-ordination Service (NCS) – Tel: 0300 3303 999
The duty consultant at the MTC should be made aware of any major trauma patients taken to a TU, via the Network Co-ordination Service.
| 12.a.iv • | Transfer of major trauma patients from a Major Trauma Centre back to a local trauma unit or rehab provider |
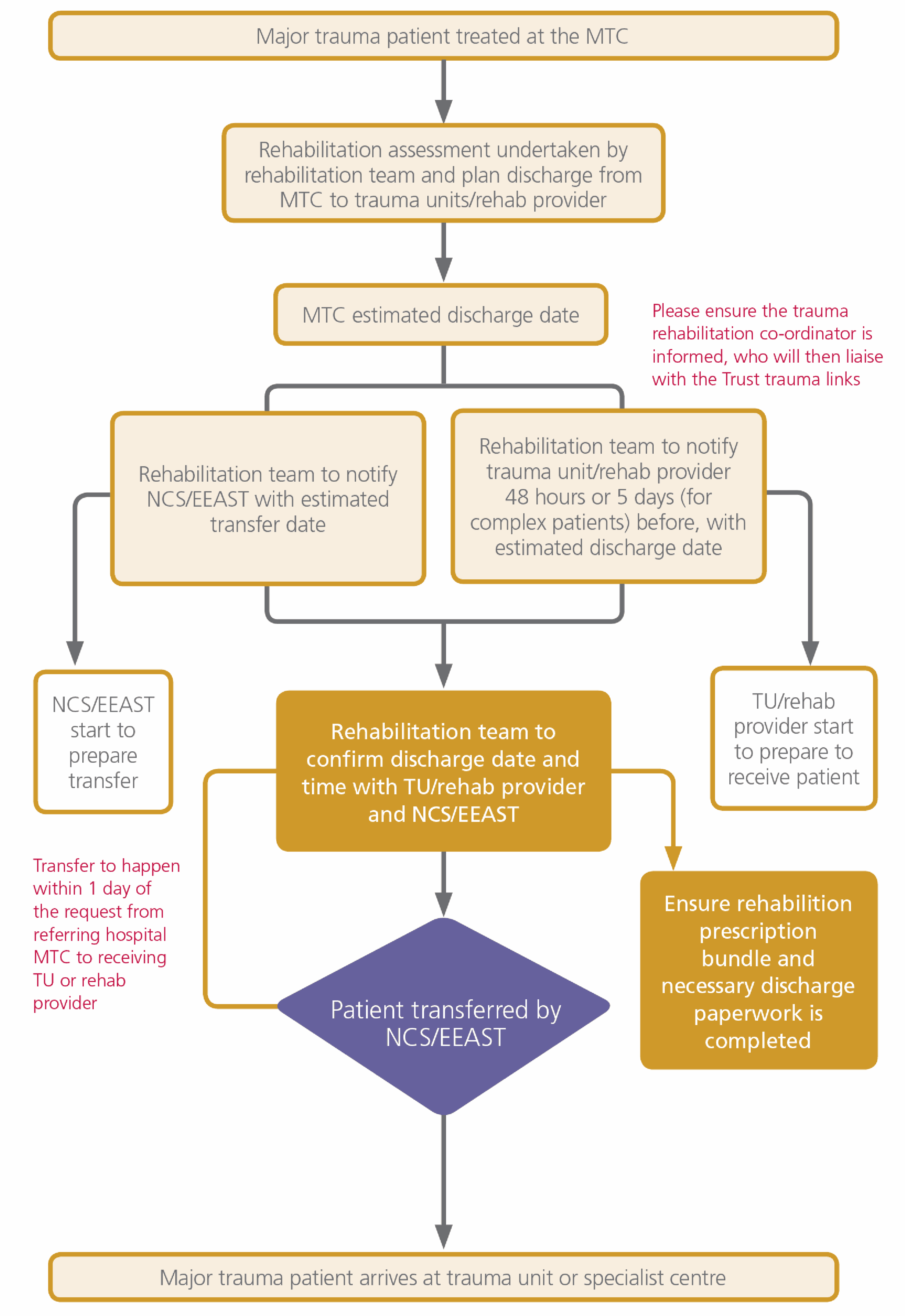
- In order to ensure the patient receives the right care in the right place appropriate
to their needs and to manage patient flow, it is important to ensure that for
patients whose specialist needs have been met, or can be met in a hospital closer
to their home, transfer out of the MTC takes place in an appropriate time frame.
Where a major trauma patient is to be discharged from a specialist centre the
same will apply.
This ‘call and receive’ protocol requires participating hospitals to accept patients who live in their catchment area from the Network whose needs can be met by that hospital. It is important to emphasise that this is not to allow the MTC to unblock beds – there has to be capability at the ‘call and receive’ hospital, not just capacity. - The agreement outlines the protocols and responsibilities for discharges from the
Major Trauma Centre (MTC), as part of the Integrated Trauma System. This will:
- ensure patients are treated at the right time, in the right place, and close to home where this is possible and appropriate
- avoid delayed discharges within the MTC, which could then impact on service capacity and capability, and consequently on outcomes
- align existing PbR and non-PbR funding with appropriate providers at each stage of the patient pathway
- Within the MTC the rehabilitation team will ensure that the patient’s pathway
through the MTC and onwards into further stages of rehabilitation and
reablement is completed in an efficient and timely fashion.
The role of this team will be to: - identify the rehabilitation needs of the patient, plan for their discharge from the moment of their admission in liaison with relevant local trauma units or rehab providers, and
- develop a prescription for rehabilitation for the patient following discharge from the MTC.
- It is not expected that this policy would apply to patients requiring critical care
(level 3). Any such cases should be agreed between referring critical care units,
and if necessary the trauma office can assist.
The ‘call and receive’ protocol:
| 12.a.v • | Summary of responsibilities to ensure effective patient flow |
The Major Trauma Centre is responsible for:
- immediately accepting primary and secondary transfers of all major trauma patients (where the ISS score is expected to be greater than 15), on the basis of immediate transfer, notification and clinical consultation
- undertaking an immediate (where clinically possible) rehabilitation assessment and providing acute and rapid intervention rehab within the acute HRG spell
- notifying the receiving hospital or other provider at least 48hrs prior to the transfer of the patient, or five days by mutual agreement where appropriate to the condition of the patient. More time may be necessary to manage the discharge of a patient with complex rehabilitation needs
- ensuring there is a clinician to clinician agreement between the MTC and receiving
team and that the patient is clinically fit to be transferred, before the 48hrs
notification time (five days for complex patients)
NB. Once this agreement is in place and the 48 hour clock has been started, if the patient is then deemed clinically unfit to transfer, the 48 hour timeline no longer applies. - ensuring that each patient has a completed prescription for rehabilitation and completed transfer discharge summary before transfer and is with the receiving team before the 48hrs notification time (five days for complex patients)
Hospital Trusts are responsible for:
- where Trusts are designated as trauma units, meeting the trauma unit standards, particularly in relation to diagnostics and clinical co-ordination of secondary transfers
- working with the MTC to support the delivery of the prescription for rehabilitation prior to the patient’s discharge from the MTC
- receiving patients discharged from the MTC, with 48hrs notice or five days for complex patients(by mutual agreement)
- taking back clinically appropriate patients where over-triage has resulted in admission to the MTC
Commissioners (CCG and NHS England, East Anglia regional Area Team) are responsible for:
- ensuring that sufficient capacity is in place, and that capacity can be flexed as necessary, to provide the range of rehabilitation, ongoing care, home placement or palliative care packages which Major Trauma patients may need
- ensuring, through contractual arrangements and individual packages of care, that patients can be received without delay, provided that 48hrs minimum notice has been provided
- working with social care providers to ensure that social needs of patients are met enabling them to move into rehabilitation settings
The Trauma Network Office (TNO) is responsible for:
- system-wide co-ordination of rehabilitation (through a network rehabilitation co-ordinator) to support the commissioning and provision of rehab and ongoing care
- alerting commissioners and providers where concerns are identified, or the system breaks down
| 12.a.vi • | Financial penalties |
Recognising the importance of optimising system wide capacity across the full patient pathway and improving clinical outcomes achieved through the more proactive provision of rehabilitation services, to minimise the risk of potential blockages to the required pathways the following additional financial penalties will be applied if there is a breach to the patient pathway.
Pathway 1 – primary transferred to the MTC
There will be no financial penalty.
Pathway 2 – secondary emergency transfers to the MTC
The ‘Call and send protocol A’ (12.a.iii) should be followed it is a clear expectation that the MTC will accept EoE major trauma patients. In the event that the MTC does not accept these patients on a frequent basis then this will be discussed with the TNO. If valid reasons are not supplied by the MTC a penalty will be introduced.
Transfer from MTC to TU or rehab provider
Where the MTC has provided the appropriate written notice, rehabilitation
prescription and transfer documentation of a patient’s suitability for discharge
(unless such clinical suitability is disputed by the commissioner or receiving provider)
and such discharge is prevented due to lack of available capacity or services, the
MTC will be entitled to make an additional charge to commissioners of:
a. £100 per bed day where the length of stay is within the relevant HRG trim point
or;
b. £100 per bed day where the length of stay is outside the relevant HRG trim point
Within the spirit of the responsibilities set out above, the MTC will be responsible for
the acute phase of the patient pathway covered by the terms of national guidance
underpinning HRGs within the PbR guidance. This includes acknowledgement of the
relevant trim points and the associated excess bed day tariff (currently £230 for all
VA HRGs).
| 12.a.vii • | Incident reporting |
All Trusts within the EoE Trauma Network will continue to operate within their own
clinical governance framework and all adverse incidents should be reported in line
with their internal governance system.
Any adverse incidents occurring during any part of the trauma patient’s pathway
should be reported in line with the Trusts internal process along with notifying the
Trust’s Trauma Committee and the TNO. All Operational Partners, Trust’s and third
sector health care providers are required to provide a summary of all of these adverse
incidents / risks on a quarterly basis to the TNO.
Due to Trust’s having their own reporting mechanisms the summary report to the
TNO should only include the below information. These can be followed up further
by the TNO if required.
Date and time of incident
Factual account of the incident
Other parties involved
Action taken or planned
Outcome
Supporting evidence if applicable
These summaries should be sent to
Trauma Network Office
Box 93
Addenbrooke’s Hospital
Hills Road
Cambridge
CB2 0QQ
Tel: 01223 349758
Email: trauma.east@nhs.net
This agreement is between:
EoE Trauma Network
| Signed | Print name | Date |
TU/Local emergency hospital
| Signed | Print name | Date |
MTC - Cambridge University Hospitals NHS Foundation Trust
| Signed | Print name | Date |
Clinical Commissioning Group: (Name)
| Signed | Print name | Date |
NHS England - East Anglia local Area Team
| Signed | Print name | Date |